Intraoperative Hyperoxia and Acute Kidney Injury
A common practice during cardiac surgery is to supply patients with increased levels of oxygen. This practice, also known as intraoperative hyperoxia, emerged in order to protect against hypoxia and precondition the heart for surgery [1]. Theoretically, hyperoxia aims to increase the levels of oxygen available to the patient, resulting in a safer procedure. Nevertheless, a recent study from the Journal of Cardiothoracic and Vascular Anesthesia found a statistically significant association between intraoperative hyperoxia and postoperative acute kidney injury (AKI) for patients undergoing cardiopulmonary bypass (CPB) [2]. Earlier works in the medical literature suggest one possible causal mechanism from intraoperative hyperoxia to AKI.
The human body uses oxygen primarily during cellular respiration, where oxygen is reduced to water. When hyperoxia causes blood oxygen levels to rise, not all of the oxygen is reduced. The excess oxygen can result in reactive oxygen species (ROSes). Examples of ROSes include peroxides, superoxide, and hydroxyl radical, all of which interfere with the basic molecules that compose human cells: lipids, carbohydrates, proteins, and nucleic acids. As a result, these compounds deplete ATP production, undermine plasma/intracellular membranes, and alter cytoskeletal structures [3].
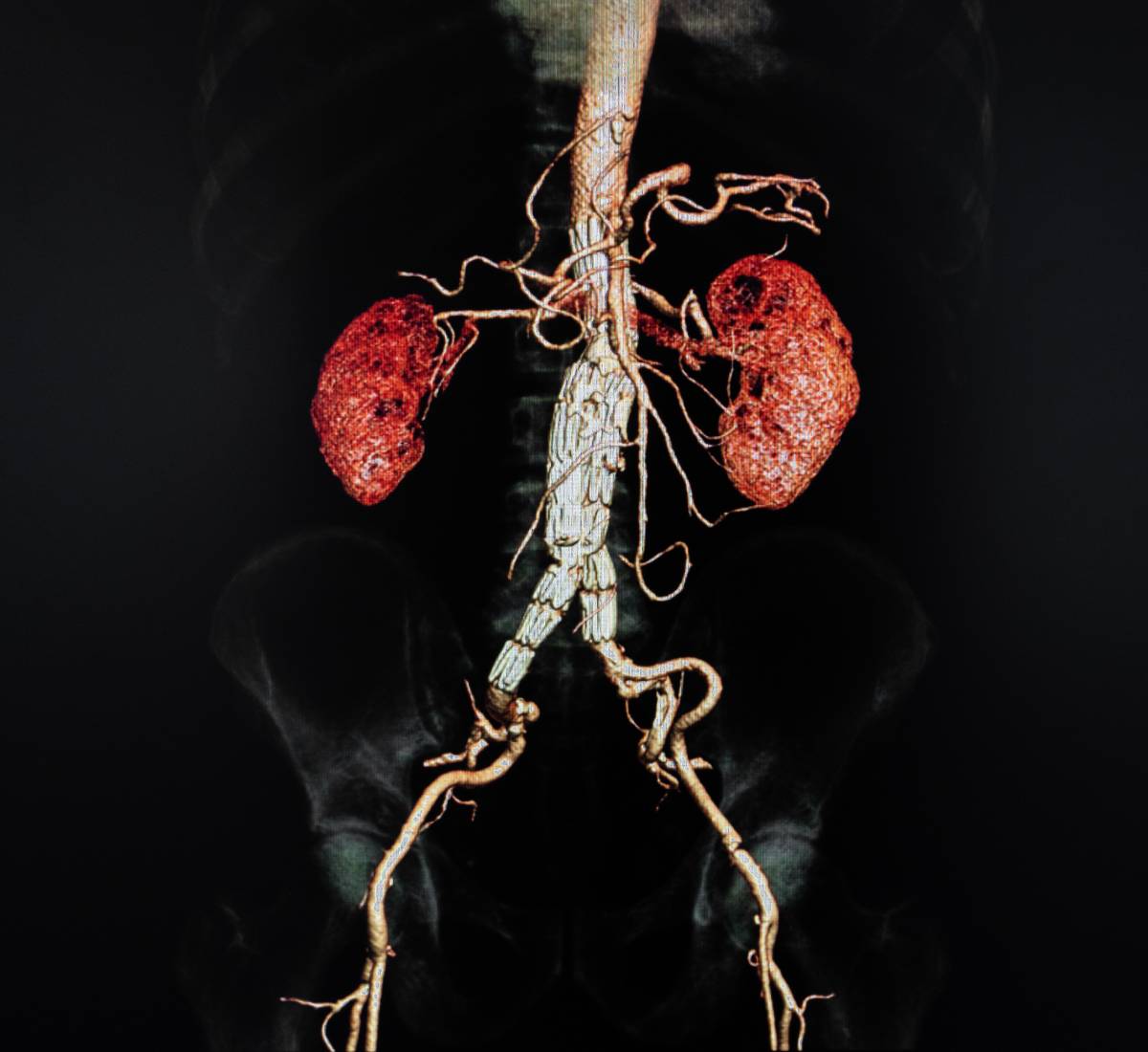
As early as the late 20th century, the kidney was known to be vulnerable to reactive oxygen species. More specifically, ROSes adversely affect the barrier function of glomerular basement membrane and the dynamics of blood flow in the kidney. ROSes may contribute to a number of kidney conditions, including AKI, renal graft rejection, acute glomerulonephritis, and toxic renal diseases [5]. With respect to AKI, they have been shown to contribute to acute tubular necrosis, one of the most common causes of AKI [3]. This evidence, backed by in vitro and in vivo animal models, suggest that ROSes are a possible cause of AKI.
Nevertheless, the literature is not conclusive on the true relationship between reactive oxygen species and AKI. A study from 2016 was only able to prove an association between AKI and the generation of ROSes, suggesting that ROSes are byproducts, not mediators, of AKI [6]. Similarly, ROSes induce an adaptive response, prompting the body to generate antioxidants and activate cytoprotective genes that might mitigate AKI and other forms of damage [3].
In conclusion, the causal connection between intraoperative hyperoxia and acute kidney injury warrants more attention from researchers. More broadly, fundamental questions remain about intraoperative hyperoxia itself, such as the optimal level of oxygen intake for post-operative outcomes [7]. For now, anesthesia providers and surgeons would be well-served to carefully weigh the risks of intraoperative hyperoxia,. For CPB in particular, studies have recommended using intraoperative hyperoxia before the procedure but not during the procedure [1][7]. In this manner, the patient’s heart should be properly preconditioned, and the patient is less likely to generate reactive oxygen species.
References
[1] Young R. W. Hyperoxia: A Review of the Risks and Benefits in Adult Cardiac Surgery. The Journal of Extracorporeal Technology 2012; 44: 4. PMID:23441567.
[2] Bae J., et al. Association Between Intraoperative Hyperoxia and Acute Kidney Injury After Cardiac Surgery: A Retrospective Observational Study. Journal of Cardiothoracic and Vascular Anesthesia 2020. DOI:10.1053/j.jvca.2020.11.054.
[3] Nath K. A., and Norby S. M. Reactive Oxygen Species and Acute Renal Failure. The American Journal of Medicine 2000; 109. DOI:10.1016/s0002-9343(00)00612-4.
[4] Boisramé-Helms J., et al. Cardiac Surgery, a Right Target for Hyperoxia? Critical Care 2016; 20: 162. DOI:10.1186/s13054-016-1347-9.
[5] Baud L., and Ardaillou R. Involvement of Reactive Oxygen Species in Kidney Damage. British Medical Bulletin 1993; 49: 3. DOI:10.1093/oxfordjournals.bmb.a072635.
[6] Ratliff B. B., et al. Oxidant Mechanisms in Renal Injury and Disease. Antioxidants and Redox Signaling 2016; 25: 3. DOI:10.1089/ars.2016.6665.
[7] Dikmen Y., and Onur A. Perioperative Hyperoxia: Perhaps a Malady in Disguise. Romanian Journal of Anaesthesia and Intensive Care 2017; 24: 1. DOI:10.21454/rjaic.7518.241.yal.
[8] Heinrichs J., et al. The Impact of Hyperoxia on Outcomes after Cardiac Surgery: A Systematic Review and Narrative Synthesis. Canadian Journal of Anesthesia 2018; 65. DOI:10.1007/s12630-018-1143-x.
